Whether speaking about using Virtual Reality to play games or to get to play doctor prior to surgery, VR is shifting how we experience anxiety, pain, surgery, fun, and games, and occasionally, these experiences overlap. To encourage the overall exposure of their VR product, this week, Sony, the Japanese multinational conglomerate, made demoing their VR gaming a free, at-home experience for selected PlayStation Plus members with a promotion offer email. The offer will be for 1,400 PlayStation Virtual Reality (PSVR) units, and this will extend just this month. The promotion is a two-week, free trial that includes the headset, a PlayStation camera (a necessary component), 2 PlayStation Move controllers, a copy of the role-playing game “The Elder Scrolls V: Skyrim VR”, and demo disc. Demo users have to provide their own PS4 game system and provide a credit card to be charged in the event that you purposefully or accidentally keep the demo unit after the 14 days, although either way, the cost is about $150 less to keep the demo package than to buy it retail. In a press release regarding a new VR experience, WarDucks of Ireland, a VR gaming and experience startup, announced the release of the RollerCoaster Legends project across multiple platforms (Oculus Rift, HTC Vive, and PSVR) for Christmas. The new experience takes on Greek mythology and icons with mythical scenes and enchanting characters along with the traditional drops and turns for players expected in a rollercoaster experience.

CEO of WarDucks, Nikki Lannen
 For example, in 2005, Australian researchers helped children who were burn-patients by using VR games during painful procedures, such as dressing changes, based on prior research that concluded that these VR games helped adult burn-patients. The perception of the nurses assisting the procedures was that the children were distracted more and cooperated more than when using just traditional pain relief medication. The VR use was not an impediment to the procedure nor in the communication with the children. From what the children reported, “The average pain scores (from the Faces Scale) for pharmacological analgesia only was 4.1 (SD 2.9), while VR coupled with pharmacological analgesia, the average pain score was 1.3 (SD 1.8).” The parents of the children concurred with the positive effects of VR for noticeably better pain management and reduced anxiety, including the children looking forward to playing the VR game. They concluded, “Intervention with Virtual Reality (VR) games is based on distraction or interruption in the way current thoughts, including pain, are processed by the brain. The study provides strong evidence supporting VR based games in providing analgesia with minimal side effects and little impact on the physical hospital environment, as well as its reusability and versatility, suggesting another option in the management of children’s acute pain.” When it comes to anxiety, in particular in regards to medical procedures, and to patient expectations and education, much research has been done to explain problems, correlations, and suggestions for corrective ideas. In 2009, US researchers presented a specific problem with patient understanding and consent and said, “Comprehension during informed consent discussions may be limited in individuals with potential language difficulty due to ethnicity or education.” In 2001, published their findings that across the studies reviewed, they discovered “the need for clinicians to clarify patients’ expectations and to assist them in having appropriate expectations of recovery”. Their conclusion was, “the understanding of the nature, extent and clinical implications of the relation between expectations and outcomes could be enhanced by more conceptually driven and methodologically sound research, including evaluations of intervention effectiveness.”
For example, in 2005, Australian researchers helped children who were burn-patients by using VR games during painful procedures, such as dressing changes, based on prior research that concluded that these VR games helped adult burn-patients. The perception of the nurses assisting the procedures was that the children were distracted more and cooperated more than when using just traditional pain relief medication. The VR use was not an impediment to the procedure nor in the communication with the children. From what the children reported, “The average pain scores (from the Faces Scale) for pharmacological analgesia only was 4.1 (SD 2.9), while VR coupled with pharmacological analgesia, the average pain score was 1.3 (SD 1.8).” The parents of the children concurred with the positive effects of VR for noticeably better pain management and reduced anxiety, including the children looking forward to playing the VR game. They concluded, “Intervention with Virtual Reality (VR) games is based on distraction or interruption in the way current thoughts, including pain, are processed by the brain. The study provides strong evidence supporting VR based games in providing analgesia with minimal side effects and little impact on the physical hospital environment, as well as its reusability and versatility, suggesting another option in the management of children’s acute pain.” When it comes to anxiety, in particular in regards to medical procedures, and to patient expectations and education, much research has been done to explain problems, correlations, and suggestions for corrective ideas. In 2009, US researchers presented a specific problem with patient understanding and consent and said, “Comprehension during informed consent discussions may be limited in individuals with potential language difficulty due to ethnicity or education.” In 2001, published their findings that across the studies reviewed, they discovered “the need for clinicians to clarify patients’ expectations and to assist them in having appropriate expectations of recovery”. Their conclusion was, “the understanding of the nature, extent and clinical implications of the relation between expectations and outcomes could be enhanced by more conceptually driven and methodologically sound research, including evaluations of intervention effectiveness.”
In 2012, Irish researchers made several key findings: “Understanding in surgical patients is poor. There is little evidence to support the use of information leaflets, although multimedia appears to be effective in improving patient understanding. The internet is not used effectively as an aid to consent by health care providers. Patients with lower educational levels may gain most from additional interventions. Improving patient understanding does not impact on their satisfaction with the treatment they have received but may reduce periprocedural anxiety. There is a need for greater awareness of patients’ information needs, and novel approaches that may enhance decision making through improved understanding are required.
This year, Indian researchers offered meta-analysis, “preoperative education reduced anxiety scores (standardized mean difference).”
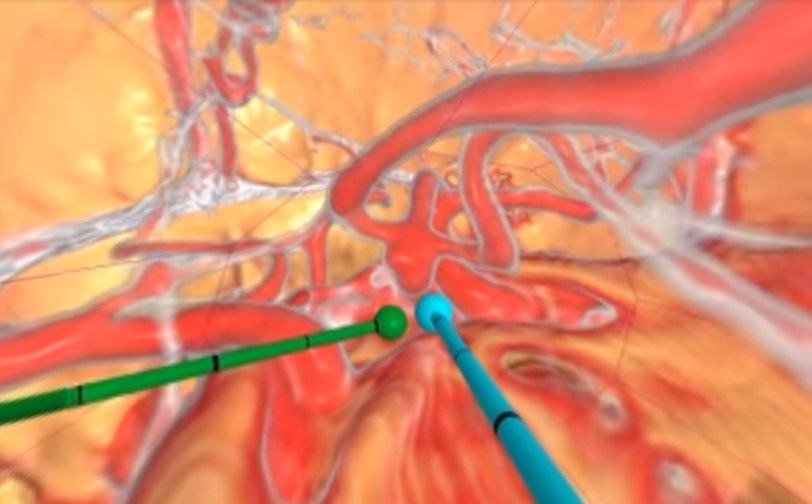
Also this year, researchers in Spain considered 200 patients waiting to undergo cardiac surgery and then reported, “Twenty-eight percent of the patients developed high preoperative anxiety” and “Both fear of the unknown and lack of information, especially related to the surgery, are crucial factors in high levels of preoperative anxiety in cardiac surgery.” In 2014, more Australian researchers examined 17 eligible trials reported data on 2689 cardiac surgery participants and then determined, “Preoperative intervention significantly reduced the time to extubation and the relative risk of developing postoperative pulmonary complications. However, it did not significantly affect the length of stay in ICU or hospital, except among older participants.” Early this year, researchers from The Netherlands offered their results on brain surgery on patients who must be awake during the surgery and said, “Awake surgery emerges as a standard of care for brain tumors located in or near eloquent areas. Levels of preoperative anxiety in patients are important because anxiety can influence cognitive performance and participation, hence altering the outcome of the procedure”. They stated, “one in every four patients reported significant anxiety symptoms in the pre-operative phase. Besides gender and age, none of the other demographic or medical factors were significantly associated with the level of anxiety.” In 2010, an Ohio startup, Surgical Theater, was born in the VR medtech spectrum, taking traditional 2D xrary images from CT and MRI scans, then creating a patient-unique 3D file that can be viewed in VR and allowing viewers to not only see the path to the surgery site but also seeing what is in the 360 degrees around them at any moment.

CEO and Co-Founder at Surgical Theater, Moty Avisar

Co-Founder & CTO at Surgical Theater, Alon Geri

Program Manager, Stanford Neurosurgical Simulation & Virtual Reality Center, Malie Collins

Chair of Neurosurgery at Standford University, Gary K. Steinberg MD, PhD

Ricardo Lockette: By Mike Morris (Flickr)

CEO of Nexeon MedSystems, Will Rosellini

Surgical Theater’s VR STudio for medical students